So…where were we? Ah, yes. Before the editorial expression of concern and the Chase debacle, we were talking about sleep.
For years and years now, I’ve been progressively increasing the number and amount of drugs I take for sleep. Frankly, the volume of pills I take for this is alarming – when I pile them up at the beginning of the night, it does rather look like I’m trying to do myself in. So when I say “I can’t sleep,” I don’t mean like “I need an occasional Ambien” or “It takes a bit longer than it does for most people.” I mean I cannot get a moment of rest without major pharmaceutical intervention. But I didn’t really know why this was the case until my most recent appointment with Dr. Cheney.
By the time my appointment rolled around this spring, I was at the maximum level of some of the things I was on, and some nights the whole regimen still wasn’t working. I had tried a couple new drugs and had not been able to tolerate them. This was part of why I moved my appointment to April from its usual spot in May – I seriously needed help figuring out what else might work. But let me back up a minute here.
When I was crashed for the second time in two months at the end of January this year (both times because of my sleep drugs failing), I asked Dr. Cheney what I could do to try to help myself bounce back faster. One of the things he suggested to me was that I could increase my inosine. I added some at night, instead of upping the morning dose, and found that it helped me sleep. So I shifted the first dose to the evening and the second to the early morning, at the same time I take my second round of things that help me sleep.
When I went to see Cheney in April, I asked him why inosine helped my insomnia. He explained that inosine produces uric acid, which scavenges peroxynitrite. Peroxynitrite, he told me, is produced in a cytokine storm in the brain, which, among other things, is a mechanism of sleep disturbance. Blocking that cytokine storm with inosine, then, helps me sleep.
This lead him into a further discussion of cytokine storms and what else counters them. Artesunate is an NF-kappa B inhibitor, and it sits at a choke point for a cytokine storm, so it should help with sleep as well. Low dose naltrexone, which I’m also on, can inhibit the cytokine synthesis of microglial cells, and encourages the body to produce its own opioids, both of which interfere with the cytokine storm.
So the fact that inosine and LDN, both of which I’d tried before my appointment and both of which helped me sleep, indicated to Dr. Cheney that a significant part of my insomnia was caused by a cytokine storm in the central nervous system. The cytokines in the central nervous system, he then explained, come from those previously mentioned microglial cells.
After that, Dr. Cheney explained what else he thought was behind my insomnia. He said that if we did a MRSI (magnetic resonance spectroscopy) scan of the brain, it would indicate what is called a lactate peak in the lateral ventricles of the brain, which should not be present, but commonly is in ME/CFS.
Interestingly, Dr. Cheney said a lactate peak in the brain is associated with both feelings of anxiety and sleep disturbances (I can’t currently find a cite for the latter). I asked him if this could help to explain that feeling I had in Chicago in 2004 that something terrible was about to happen. He remembered that being part of my case and said indeed, a feeling of doom would be consistent with that physiological symptom.
Because my body is running in a low-energy state because of loss of mitochondrial function, he went on to say, it isn’t producing enough ATP for my brain. So, to compensate, he said, my brain is partially running on adrenaline – and it’s rather difficult to sleep when one’s brain is running on adrenaline.
And if there’s a problem with mitochondria, he told us, there will inevitably be a problem with magnesium depletion. So supplementing magnesium should help with sleep, and a number of other problems as well. (And it did, as I mentioned in the previous insomnia entry.)
So: Inosine, LDN, and magnesium have all helped. I’m not sure whether the artesunate at night is helping, but it doesn’t seem to hurt. The other thing that I discovered that helps – and this happened entirely by accident – is calcium. One night when I overdid it on the betaine (the stomach acid supplement), I chewed some Tums to knock the acid down, and found it was easier to sleep. I know magnesium improves the absorption of calcium, so perhaps taking the two together (they’re often paired in mineral supplements) is having a synergistic effect. Also, over the course of the night, every time I realize I’m awake, I dose myself with several sprays of ionic magnesium, and that definitely seems to help me fall back to sleep more quickly.
At this point my sleep cocktail includes a half-dozen prescription drugs – but none of them are traditional sleeping pills. This is because Ambien and the rest of the “z-drugs” are closely related to benzodiazapines, and they do the same thing to me that the benzos do: give me screaming anxiety.
I’m at the maximum dosage of the last two, Soma and Remeron. I tolerate all of these pretty well, though I take a beta-blocker because the Seroquel tends to run my heart rate up. I take all of these with that previously mentioned betaine, because I produce little stomach acid of my own and I won’t absorb the pills without it.
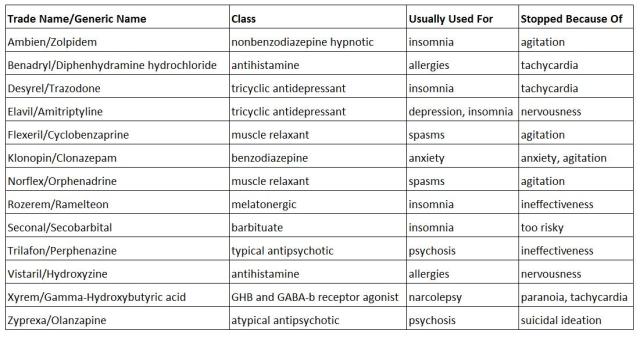
And here are the things I’ve tried and abandoned for various reasons. For the purposes of this table, nervousness < anxiety < agitation. There’s a whole lot of not fun here.
If the current wheelbarrow full of pills stops working, we have Phenergan, an anti-nausea medication, on deck to try.
I’m very grateful there are as many pharmaceuticals to try as there are, and that Dr. Cheney knows the world of supplements so well. Without any sleep drugs, I would have died in 2008. Because I have them, and Dr. Cheney’s expertise, I’m not only still here, I’ve actually improved since first seeing him in 2009. Back then, my dream was just being able to read on the computer for the whole day. Now I can even type a little most days. Sure, I’m not where I wish I could be, but I never thought I would get back even as far as I have. I’m happy to have it, for however long it lasts.
May 2013 update: I’ve added two supplements to my nightly regimen this year – P5P and Sam-e. I’m taking them in the wee hours and they’re helping me stay asleep for the second half of the night.




Two things:
Serious sympathies on your insomnia. I have ME/CFS and I know the sleep disturbance is exquisite torture. I hope things continue to improve.
I have a dog named Bootsy (Collins) and another Maceo (Parker), my husband named them. But it did make me smile to see your very cute kitties’ names 🙂
Best wishes,
Penny
Thanks, Penny. Yes, the insomnia is a whole lot of not fun.
Too funny that you also have a Bootsy! A friend was puzzled when he finally met Boots…he said, “But he doesn’t have any boots!” He had never heard of Mr. Collins. So we enlightened him.
Truthfully, my husband is the jazz fan, though we both like funk music. When we adopted Ming and Cole, he got to name the boys, and I named their mother Beauty after a poem by Eve Merriam. Beauty has passed on now, but she was the mirror image of Coltrane – black and white, with a spot over her right eye. She was delightfully grouchy and loved Chimp but barely tolerated me. She had a habit of swiping at me when I would try to pet her. I liked to say to her in a baby-talk voice, “Who rescued you and your kittens out of the storm drain. Who? Oh, you don’t care, do you? No, you don’t care!” Her poem:
The Stray Cat
It’s just an old alley cat
that has followed us all the way home.
It hasn’t a star on its forehead
or a silky satiny coat.
No proud tiger strips, no dainty tread,
no elegant velvet throat.
It’s a splotchy, blotchy
city cat, not a pretty cat,
a rough little tough little bag of old bones.
“Beauty,” we shall call you.
“Beauty, come in.”
***
Maybe she was nasty to me because she felt insulted!
That’s a great poem! We have a grouchy ex-stray kitty too, she is affectionate and wants to be in my lap at all times, but is quick to register her displeasure at any unnecessary movement – lucky for her fidgeting isn’t something I do much anymore 🙂
Isn’t it interesting how we don’t fidget? That’s what I see as the mark of someone with serious ME/CFS – do they gesture while they’re talking? If so, they are probably functioning pretty well with it.
I know how hard it is to get good sleep. I have CFS and so many other things, including sleep distrubance. Thank you so much for sharing this information. I was wondering how to read your Part I, I would like to read that too.
I am trying a Delta Wave CD, that seems to be helping a little. Continue prayers for your health and good sleep.
Welcome, Nan! Thanks for your sympathies. I linked Part I above the picture in this entry – you can also find it by clicking here: Part I.
Oh, after I send you an email, I looked again and saw that I could post. This is why I can’t do more advanced Internet stuff, my brain is full already.
No worries, Kathy! Mine’s running at less than half speed too.
Thank you very much again for all the information you are putting out for us “weapon – graders”.
Thank God that at least one physician , Dr Cheney, tries to understand and treat it for what it is.
My physician comes from the fibro angle of too much arousal in the brain and prescribes accordingly. That would fit with the brain running on adrenalin but of course he did not make the connection with not enough ATP and magnesium depletion – and the cytokine storm due to damaged micro glia cells – and guess why they are damaged? XMRV or some other HGRV.
I just ordered some inosine to add to my regime. The phenergan is a sedating antihistamine which we can get here ( UK) OTC. One of the first things I tried. It works to start with but tolerance builds up quit fast and gave me headaches when I went up with the dose. But of course I have not tried it in combination with other things. It might work synergistically. I hope it helps you.
I also tried the magnesium spray and it works fine to fall asleep when waking up at night – but only in a mild excitatory state. When it comes to the proper excitatory storm only heavy duty double dose of one or the other chemical of choice does the job – and every night a different one!
That’s what I meant with ROTATION in my previous response to your post PART 1. My theory is that if we rotate the heavy duty chemicals there is less chance to reach the maximum dose and the need to find something else. Also, if something really stops working it might work again in one or two years time.
I never in my life want to relive that week in 1999 when I could only doze one or two hours per night and ended up in a relapse that send me on a downwards spiral which although now slowed by the sleep cocktail I take, has not phased out.
I am 62 and had moderate to severe ME for 23 years , so this might be expected but I think with your being younger and shorter duration of illness Dr Cheney might give you the chance for a reasonable amount of recovery. I sincerely wish this for you to happen.
23 years, Inge? Holy cats. You really are a veteran.
It’s very interesting that your doctor also subscribes to the idea of too much arousal. I think there must be something to it.
Do let me know how you get on with the inosine. I hope it will be helpful.
Glad to hear that the magnesium spray gave you some benefit. Yes, it is a helpful supplement, but it does not do the real heavy lifting of knocking the brain out so we can sleep.
I agree, I never want to go through the totally not sleeping ever again. It is such awful misery.
And thanks for the well-wishes…I hope we all will get recovery, soonest!
I have had this disease for 25 years and the sleep disorder has been a very major problem. I have to guard against any factors that might exacerbate it. And my body wants to sleep in the daytime. No matter what I do, I get the best sleep in the afternoons, so my life is turned upside down all of the time. Have to cancel appointments, not do errands, etc.
And as we know, not getting adequate deep sleep means more muscle pain and worse symptoms, weakness, lack of any stamina, etc. And it means one cannot go outside or do anything. I can’t take a shower without sleep or go around the corner to the store or read.
I totally sympathize with your statements about the sleep disorder. I don’t know if anyone really understands this if they don’t have it. I don’t know if doctors get it either, how bad this is.
I had surgery 10 years ago. Afterwards I did not sleep in the hospital for 10 days, nothing, not even an hour. I could not read, despite my stack of books and newspapers. I couldn’t watch tv although I paid for it and had it on. I couldn’t understand a word. And it affected my rehabilitation.
Then on day 10 I slept for 24 hours, then the hyperinsomnia started again and lasted until I left four days later. No one understands this if they don’t have this disease. I am convinced of this.
Thanks for your list and side effects. Your explanations are very good, although I sympathize with how difficult this problem is and what you have gone through.
I am very glad you have an understanding and helpful partner.
Pingback: Happy Blogiversary to Me | No Poster Girl
I know this is an old post, but just in case this helps someone.. I too lost the ability to sleep. I felt nauseous and raw the whole day and the best I could do at night was to use my fingers to keep my eyes closed. I had a polysomnogram which showed UARS (google the Stanford website for info) – basically the upper airway collapses a little during sleep and the pressure in your lungs gets out of sync. The body then wakes up to compensate.. over and over all night. I am using Cpap now and it seems to help. I fall asleep quickly and don’t feel nauseous anymore. My pain is much less and I can regulate my temperature better. I still feel tired during the day but it is a big improvement on before. I take one sleep med to get me sleepy at the right time, and after that I’m good. If you are going through the polysomnogram be sure to check they will be monitoring for UARS alongside everything else. I feel like this has been one of the puzzle pieces for me, let’s hope we can find the others. Wishing you well.
I forgot.. since starting the treatment my blood pressure has gone up to a normal level, what a difference. My bp has always been in the dumps – I just thought everyone felt dizzy, had their vision go black and such. Doh! I wonder if all that time with low pressure is somehow in the mix-does it mean that my body was under stress from not enough o2 getting about/co2 not being cleared? Who knows..
Thanks for the comment, little miss. I had a sleep study done early on in the disease, and my airway was without problems. Dr. Cheney is pretty certain that the problem is an ATP deficit and my body overproducing adrenaline as a result. Glad to hear you found something that works for you!
Pingback: My Weapons-Grade Insomnia | No Poster Girl
How do I contact Dr Cheney for sleep help. I am taking over the counter Power to Sleep PM. What can I do?
Judy, I just saw your question now. You would have to become a Cheney patient, which is a pretty big undertaking – his office is in Asheville, NC, and a patient’s first visit to him is a two-day one. If you are interested in seeing him, the clinic website is here and has contact info. You can call and speak to his assistant, Dixie, and she can start the ball rolling for you. I’m sorry there isn’t an easier way to get a consult – I know it’s a big commitment.
Pingback: New Bottle Paranoia Syndrome | No Poster Girl
Hi, I have severe M.E and severe insomnia. I take a cocktail of meds too, though not as much as you. I’m keen to know how the inosine works and how much to take and if there are any precautions with it? I live in New Zealand and we don’t have as many medications available here, I can’t even get inosine! I’ve been having excruciating sleeplessness for the past year where the drugs aren’t working. Sometimes I get some sleep and other times I go days without any. The longest time i’ve been without sleep was a period of about 3months, I lost all function of my body and mind. I’m glad you’re on the right mix of meds and supplements now. I am desperate to try anything!! X
Hi Stacey – I’m terribly sorry, but I didn’t see this comment until just now. Inosine works, Dr. Cheney says, by interfering with cytokine storms in the brain. I take 1000 mg at bedtime and another 1000 mg in the wee hours of the morning. The only precaution I know of with it is that it can raise uric acid levels, which can cause gout if you’re prone to that. Hope you are doing better now than when you left this comment.
Pingback: Brain No Go So Good | No Poster Girl
You can still get Seconal?
You can, but it’s not easy. When we were living in California, our local pharmacy didn’t carry it; they needed to get it from San Francisco.
Muscimol supposed to work for slow wave sleep with less addiction, but Merc stop making it (because it works you know what I mean?) And now selling the trade of this medicine to 101 with new name Gaboxadol. Not yet nold but not for insomnia, but other brain disorder syndrome.
People here been tested for Lyme disease?
I’m also wondering if anyone on here has been tested for Lyme disease. I have it, and have the exact same symptoms as far as sleep goes. Nothing works, even klonopin. I know of others who have Lyme and had their insomnia go away with really good Lyme treatment.
Had Lyme disease years ago (2004), cured by natural doctor with intense herbal, vitamins and colloidal silver.
Now I have Fatal Insomnia after treatment of high dose fluoroquinolone antibiotic that damage tissue/cells/neurons, CNS, Supra Chiasmatic Nucleus, Pineal gland and Spinal Cord. Of course this fluoroquinolone also damaging many other part in my body but the ones above is the condition that terminate my sleeping regulator. Sleep never established any longer and in a good night benzo could only make me sleep not more that two hours with nightmares beside making my whole condition get worst, short breath, painful neural sensations, anxiety.
Sorry to hear that, jiwa.
Many people don’t realize that their severe insomnia cause by their other medical course in the past to treat other condition. Fluoroquinolone alone for example could damage Central Nervous System, especially when it mixed with NASAID and the adverse reaction and damage could happened in a months to a years later.
Thankfully, I’ve never been on a fluoroquinolone. Just got lucky other ways!
What about Inosine Pranobex? Different thing?
Yes, it’s a different thing.